Genetics
"Genetics" means relating to a person’s genes and what they have inherited. Genes are responsible for our traits and unique characteristics. In spinal muscular atrophy (SMA), there is a mutation in a gene responsible for a protein that is critical to the function of the nerves that control normal muscle movements.
SMA and Genetics
Spinal muscular atrophy (SMA) is caused by a mutation in the survival motor neuron gene 1 (SMN1). In a healthy person, this gene produces a protein—called survival motor neuron protein or SMN protein—that is critical to the function of the nerves that control our muscles. Without it, those nerve cells cannot properly function and eventually die, leading to debilitating and sometimes fatal muscle weakness.
Most people have two copies of the SMN1 gene. SMA occurs when both of an individual’s SMN1 copies have missing or mutated segments. Except in very rare cases, this happens when that individual has inherited two faulty copies of the gene—one from each parent. These parents do not have SMA themselves but are said to be “carriers” of SMA. Read more about this in our Care Series Booklet on the Genetics of SMA.
The SMN2 Gene
A second gene also has a role in producing SMN protein. This is the survival motor neuron gene 2 (SMN2), often called the SMA “back-up gene.” Most of the SMN protein produced by SMN2 lacks a key building block that is normally produced by SMN1. This means that SMN2 cannot fully make up for the mutated SMN1 gene. The number of SMN2 genes can vary from person to person, and individuals with more SMN2 copies usually have a less severe form of SMA than those with fewer copies. However, the number of copies of SMN2 does not reliably predict the severity of SMA symptoms an individual will have or how weak their muscles will become.
One potential treatment for SMA is to cause SMN2 to produce more protein. Another is to change how the protein is produced so the SMN2-produced protein contains all the key building blocks needed. Cure SMA’s comprehensive research program explores these and other possible SMA treatments.
What It Means To Be an SMA Carrier
Individuals who have one faulty copy and one functioning copy of SMN1 are called carriers. Carriers do not have SMA, but they may pass the faulty gene on to their children. Approximately one in 50 people is a genetic carrier for SMA. Many times, carriers do not know they are carriers until they have a child born with SMA.
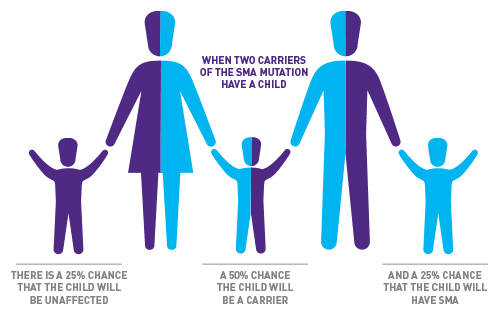
- When two carriers have a child, there is a 25% chance that the child will be unaffected, a 50% chance that the child will also be a carrier, and a 25% chance that the child will have SMA. This risk is the same for each pregnancy
- If only one parent is a carrier, the child is usually not at risk for SMA, though they do have a 50% chance of being a carrier themselves. However, in very rare cases, spontaneous genetic changes in the SMN1 gene can occur during egg or sperm production, causing the child to have SMA even though only one parent is a carrier
In addition, a very small percentage of carriers have genetic changes that cannot be identified through current testing technology. In this case, it will appear as though the disease has been caused by a single carrier.
Carrier Testing
A DNA test is the only way to know if a person is a carrier of the SMA gene. The DNA test is a simple procedure, done through blood or saliva testing.
In the general population, this test can detect about 95% of carriers. However, in African-American populations, detection is closer to 70%. This is because a difficult to detect mutation is seen more frequently in African-American populations than in other races.
The American College of Obstetricians and Gynecologists (ACOG) recommends that all women who are thinking about becoming pregnant, or who are already pregnant, be offered carrier screening for SMA and other genetic conditions. If the woman is a carrier, her partner can then be tested.
In addition, individuals with a family history of SMA are often encouraged to have carrier screening. Deciding whether or not to undergo genetic testing is highly personal, and we strongly recommend discussing it with a physician or genetic counselor.

Reproductive Choices
For couples who are carriers, reproductive decisions can be sensitive. A number of options are available such as no testing, prenatal testing, adoption, and pre-implantation genetic diagnosis (PGD). PGD screens embryos for genetic disorders and selects the unaffected embryos for implantation.
Cure SMA believes that everyone has the right to choose whatever option is best for your own values. We help people understand their options and provide resources to support their decisions. We do not advocate any specific course of action, nor do we pressure anyone to choose one way or the other. We encourage each person to discuss their situation with a physician, genetic counselor, and—if helpful—a therapist or spiritual advisor.